BMI: An Outdated Measure of Health
Ever been to a doctor’s office and the first thing you see on the wall is the massive BMI chart above the old outdated scale?!
For most people, being weighed and measured is the first thing that happens during a doctor’s appointment. From a person’s weight and height, the doctor can calculate a number called their Body Mass Index (BMI), previously otherwise known as Quetelets Index.. This number is used by doctors to estimate how healthy a person is, and doctors will often give lifestyle recommendations to patients based on this number.
However, whether or not BMI should be used as a tool to measure a person’s health has been a topic of debate for years. Evidence suggests that BMI is a poor measure of health and does not accurately predict health risks in individuals. Despite this evidence, BMI is still used in almost all doctor’s offices across America.
So, let’s talk about it! What exactly is BMI? How is it used? Why is it controversial to use it to measure health?
What Is BMI?
BMI is used to determine a person’s body weight category based on height and weight measurements. Typically, the higher a person’s weight is, the higher their BMI will be. An individual’s BMI will fall into one of four categories: underweight, normal, overweight, and obese.
BMI was created in the 1830s by a scientist named Adolphe Quetelet, which is why you may have heard BMI referred to as “Quetelet’s Index”. Quetelet was an astronomer and mathematician, not a medical doctor. He created BMI to classify people for his own research, and had no intention of using it for medical or diagnostic purposes. Yes you read that right, and read it again to let that sink in.
Skipping ahead to 1972, a psychologist named Ancel Keys (also not a healthcare professional!) published a journal article about why BMI was the best way to estimate body fat when compared to other methods of measurement. From here, doctors and insurance companies quickly adopted BMI as a tool to estimate health risks in clients.
Adding to the timeline, in 1998, the National Institutes of Health decided to lower the overweight category of BMI from 27.8 to 25. Because of this adjustment, millions of people whose BMIs were categorized as normal were suddenly considered to be overweight. However, this amendment sparked a lot of criticism. The change to the BMI threshold for the overweight category was influenced by the International Obesity Task Force. This organization was funded heavily by companies that manufactured weight loss drugs.
The implication of the International Obesity Task Force being funded by weight loss drug manufacturers is a heavy one! The goal of these weight loss drug companies would have been to increase their profits. What better way would there have been to do so than by increasing the number of American citizens who are classified as overweight? It is very likely that these drug companies used their financial influence over the International Obesity Task Force to lower the overweight category of BMI. However, it is important to recognize that there is no hard evidence of this influence, no matter how well it lines up.
The change in the BMI overweight threshold led doctors to tell more people that they needed to lose weight. During this time, dieting and diet pills were far more accepted than they are today. Consequently, this created the perfect storm to push more people to buy weight loss pills, which was most likely the intention of the weight loss drug companies who were financially associated with the International Obesity Task Force. Therefore, all of this is crucial evidence that lowering the overweight BMI threshold was a profit driven, scientifically shaky decision made with little regard to how it would impact people all around the globe.
To further showcase that the lowering of the overweight BMI threshold was a poor decision, let’s take a look at the association of mortality with being overweight/obese according to BMI categories. A 2013 systematic review study found that people who were classified as overweight by their BMI were associated with having significantly lower all-cause mortality risk. Additionally, those classified with class one obesity (BMI= 30 to <35) did not have an association with having a higher mortality risk. These findings directly contradict the popular assumption that being overweight/obese are direct risks to one’s health.
Why is BMI used today?
BMI is the most widely used estimate of individual health because it is inexpensive, non-invasive, and quick. It is currently used in healthcare to assess a person’s risk for health problems, such as type 2 diabetes, cardiovascular disease, hypertension, and more. A doctor will presume that you are at a higher risk for developing these health problems if your BMI is classified as “overweight” or “obese”.
Problems With BMI
BMI sounds so simple, doesn’t it? Your weight and height can be used to tell you how healthy you are, right? Wrong.
Recently, we have learned that SO much more goes into ‘being healthy’ or “being at risk for health problems” than BMI. Science suggests that body fat distribution, weekly physical activity, genetics, diet, and more are all key contributors to general health. Notice… these factors have nothing to do with weight specifically! Having a BMI on the lower end of the spectrum does not mean that you are immune to developing health problems, and having a BMI on the higher end of the spectrum does not mean you are going to develop a health problem.
All that being said, BMI has many flaws. Firstly, the author of BMI used the heights and weights of White men in the creation of the BMI equation. This means that the data Adolphe Quetelet analyzed to create the BMI formula did not take other races or genders into account. Today, we know that body composition varies widely across different ethnicities. How can a standard created from the data of White men in the 1800s be accurately applied to people of different ethnicities, races, and genders?
Another major flaw of BMI is its failure to measure body composition. BMI uses weight and height to categorize people into health categories, but body composition is a better indicator of fitness and health risk according to recent research.
For example, there are many athletes who are classified as obese/overweight by their BMIs such as The Rock, Arnold Schwartzenager, and Tom Brady. However, I don’t think that anyone would consider these athletes to be “unhealthy”. When considering body composition, these three athletes have a lot of lean body mass and sturdy bones. Lean body mass and strong bones go hand in hand! Having greater amounts of lean body mass works to keep your bones strong and prevents them from thinning. Both lean body mass and strong bones are forged from health promoting behaviors such as regular physical activity, muscle strengthening exercises, and consuming a balanced diet.
Body composition measures fat-free mass and fat mass to estimate health. Having a greater proportion of fat-free mass and a lower proportion of fat mass is correlated with improved general health and decreased risk of developing health problems.
It is important to emphasize here, correlation is not the same as causation. Having a higher body fat percentage does NOT mean that you will develop a chronic disease and having a lower body fat percentage doesn’t mean that you won’t. Period. Failing to recognize that larger bodies are not the cause of individual health problems (causation) is part of the mindset that perpetuates weight stigma and fatphobia today. As I said previously in the article, BMI and weight cannot be used to make a judgment of a person’s general health.
Additionally, even though studies examining the link between body composition and health risks tend to be more slightly inclusive than BMI, they still do not routinely include diverse populations in the data that they use to extrapolate conclusions from. Because of this, the applicability of these studies on all ethnicities, races, and genders is still questionable.
Lastly, you cannot possibly have a conversation about health without discussing the Social Determinants of Health (SODH).
According to Healthy People 2023, SODH are defined as “the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks”. Examples include education, income, discrimination, access to transportation, having a safe place to live, pollution levels, and access to nutritious food. It has been established that SDOH are widely responsible for the health disparities and inequities that affect millions of Americans today. Notice that a large degree of these domains are out of one’s control.
Because SDOH are out of a person’s immediate control, at least part of a person’s health is out of their control as well. For example, a person with a relatively lower BMI living in an area with high levels of air pollution could regularly eat nutrient dense meals, avoid smoking, and be physically active… but their overall health would still be negatively impacted by the air that they breathe. In this way, a person’s health is harmed despite the health-promoting behaviors that they regularly practice. This shows yet again how you can’t evaluate someone’s health by their body size or BMI.
The Takeaway
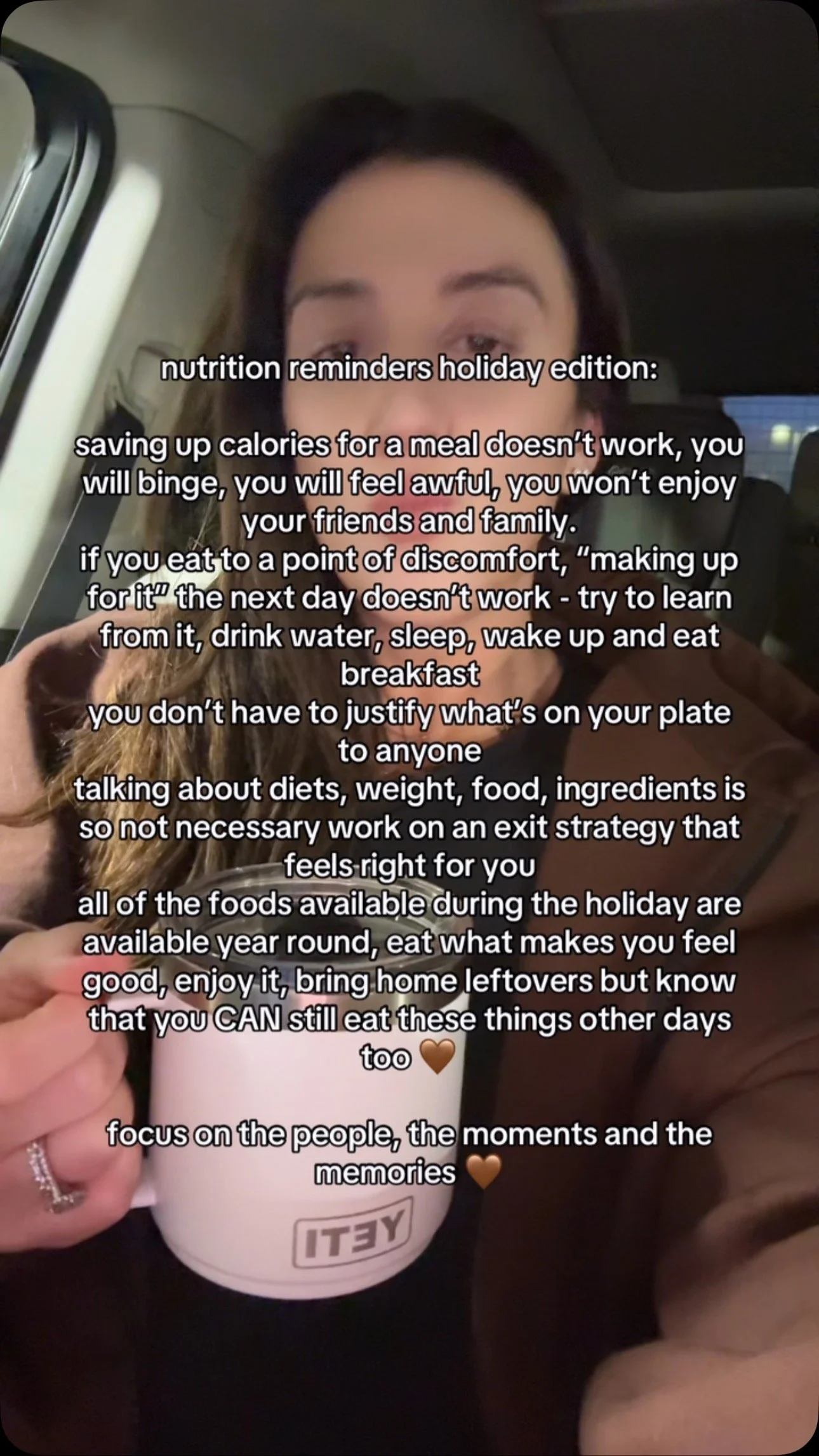
If your BMI is a source of stress for you, take care to remember that this number does not define your health. Health & Wellness is made up of so many different factors (daily habits, caring relationships, mental well-being, socioeconomic status, access to unbiased medical care, etc.) and it is impossible to boil it all down to something as simple as a single number. All bodies are good bodies, and all bodies can be healthy regardless of BMI or weight. Be kind to yourself.
If improving your life through health promoting behaviors is something you’re interested in, learn about our nutrition coaching offerings!
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4890841/
https://www.sciencedirect.com/science/article/pii/0021968172900276
https://www.endocrineweb.com/news/problems-with-BMI
https://www.verywellhealth.com/bmi-measurements-non-white-population-5185655
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8399582/
https://jamanetwork.com/journals/jama/fullarticle/1555137
https://www.motherjones.com/politics/2014/08/why-bmi-big-fat-scam/
https://health.gov/healthypeople/priority-areas/social-determinants-health
Written by Sarah Haaser
Hey, I'm Sarah!
I am an undergraduate senior at Purdue University majoring in Nutrition & Dietetics. I enjoy trying new recipes and thrifting when I’m not in class or studying! Learn more about the HSH offerings here.








































February is American Heart Month, and as a registered dietitian, I want to share my secret heart-healthy tip with you: consider adding Florida Orange Juice to your daily routine!